Publication | A Journey to the Central Nervous System: Routes of Flaviviral Neuroinvasion in Human Disease
This publication is part of the project ‘Preparing for vector-borne virus outbreaks in a changing world: a One Health Approach’ (NWA.1160.1S.210) which is (partly) financed by the Dutch Research Council (NWO).

Authors: Eleanor M. Marshall, Marion P. G. Koopmans and Barry Rockx
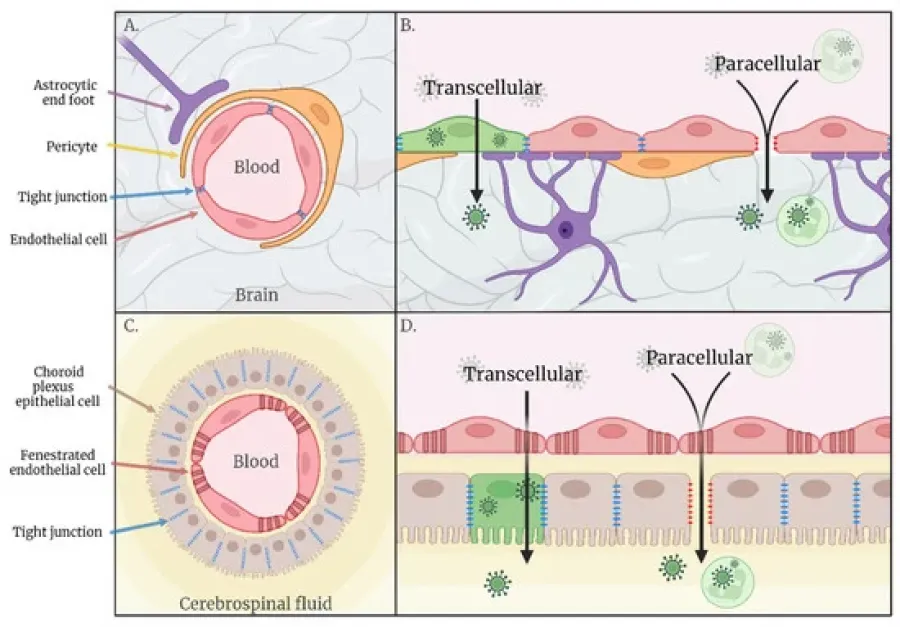
Many arboviruses, including viruses of the Flavivirus genera, are known to cause severe neurological disease in humans, often with long-lasting, debilitating sequalae in surviving patients. These emerging pathogens impact millions of people worldwide, yet still relatively little is known about the exact mechanisms by which they gain access to the human central nervous system. This review focusses on potential haematogenous and transneural routes of neuroinvasion employed by flaviviruses and identifies numerous gaps in knowledge, especially regarding lesser-studied interfaces of possible invasion such as the blood–cerebrospinal fluid barrier, and novel routes such as the gut–brain axis. The complex balance of pro-inflammatory and antiviral immune responses to viral neuroinvasion and pathology is also discussed, especially in the context of the hypothesised Trojan horse mechanism of neuroinvasion. A greater understanding of the routes and mechanisms of arboviral neuroinvasion, and how they differ between viruses, will aid in predictive assessments of the neuroinvasive potential of new and emerging arboviruses, and may provide opportunity for attenuation, development of novel intervention strategies and rational vaccine design for highly neurovirulent arboviruses.
1. Introduction
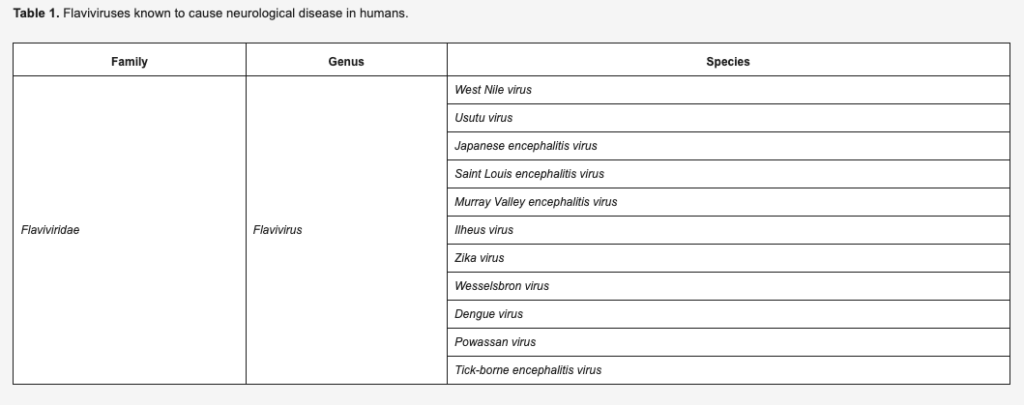
In recent years, geographical expansion of arthropod vector populations due to climatic changes, and intrusion of human populations into sylvatic cycles of transmission as a result of increased urbanisation and population growth, has fuelled an increased risk to human health posed by arthropod-borne viruses (arboviruses) [1]. Arboviruses depend upon invertebrate vectors such as mosquitoes, ticks and sandflies for transmission between enzootic hosts, with humans often acting as incidental dead-end hosts. Many arboviruses are capable of causing severe neurological disease in humans, including members of the Flavivirus genus (Table 1). However, the mechanisms by which many new and emerging arboviruses gain entry to the central nervous system (CNS) to cause neurological disease, are poorly understood.
Identifying the threat posed to humans by emerging arboviruses with neuroinvasive potential is difficult because the majority of cases are mild or asymptomatic, leading to many individuals not seeking clinical care or being diagnosed with infection of a specific pathogen. In the event of severe disease or case lethality, the disease stage is too advanced to recognise initial routes of CNS invasion. In addition, regions of interest for studying neuroinvasive routes such as the choroid plexus, sciatic nerve and the olfactory epithelia, are often not investigated post mortem. Therefore, in vitro and in vivo model systems must be used to study the initial stages of disease progression and neuroinvasion and be extrapolated to the much more complex physiological setting.
The current lack of basic understanding of how, and why, arboviruses gain entry into the CNS prevents rapid identification of novel viruses with neuroinvasive potential and hinders clinical diagnoses. Therefore, the aim of this review is to provide an overview of arboviral neuroinvasive mechanisms, with a particular focus on flaviviruses, to aid the direction of future work by highlighting gaps in current knowledge and ultimately support development of targeted interventions, vaccine design and public health preparedness for current and future emerging neuroinvasive viruses.
Here, we review the two main proposed routes of arboviral neuroinvasion: the haematogenous and transneural routes.
Source: MDPI
Date: september 15th 2022